Scientists from Yale University have developed a new class of glioma and glioblastoma (GBM) drugs that exploit tumors that lack the DNA repair enzyme O6-methylguanine methyl transferase, or MGMT. The drugs lead to the generation of cytotoxic DNA that selectively killed tumor cells in several in vivo mouse models of drug-resistant GBM without significant off-target toxicity. The new approach relies on direct DNA modification to exploit specific DNA repair defects and combat drug-resistant tumors.
Results of the study are published in Science.
About half of GBMs and two-thirds of grade II and III gliomas lack MGMT. These cancers initially response to treatment with the drug temozolomide (TMZ) but drug resistance eventually develops in most patients through the loss of the mismatch repair (MMR) pathway.
“The problem is that there’s a resistance mechanism which involves further alterations in DNA repair,” said co-senior author Seth Herzon, PhD, professor of chemistry at Yale University School of Medicine. It involves silencing of the MMR pathway which in turn limits the efficacy of TMZ. Patients typically recur and do not respond after that initial round of treatment.
In a unique strategy, the Yale team leverages this lack of MGMT to kill GBM tumor cells selectively. “Deficiencies in DNA repair go hand in hand with tumorigenesis,” said Herzon. “Our strategy is essentially to exploit the DNA damage response to obtain tumor-specific activity.”
In collaboration with long-time collaborator and co-senior author Ranjit Bindra, MD, PhD, the team developed TMZ analogs that create a dynamic primary DNA lesion, which can be repaired in healthy cells with intact MGMT-mediated DNA repair mechanisms. However, cancer cells lacking MGMT expression cannot repair the damage.
Herzon explains the drugs transfer a small two-carbon residue with a fluorine constituent to O6 of guanine to form that primary lesion which can be reversed by MGMT in healthy tissue. “That’s the basis of our selectivity; we’re not physically just delivering into the tumor,” he Bindra. The drugs go everywhere but in healthy cells, MGMT is ubiquitously expressed, and can process that initial primary lesion and repair it. “But in MGMT-minus tumors you don’t have that reversal pathway available,” added Herzon. Consequently, that lesion then converts to more toxic secondary DNA lesions that result in the selective killing of MGMT-deficient tumor cells.
Their experiments lead to a lead candidate, KL50. “One of the reasons we were able to move very quickly with this research is that our compound is a very small change structurally from TMZ,” Herzon explains. “So it has CNS penetration, it is well-tolerated, it is orally available, and in this paper, we’ve demonstrated efficacy in vivo in intracranial models of drug resistant GBM.”
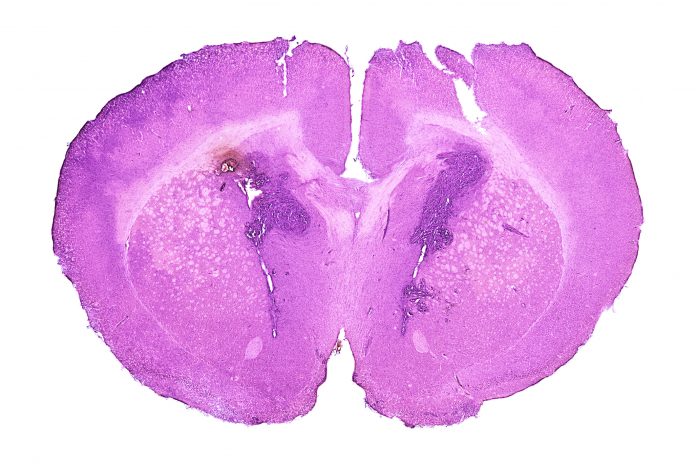
The researchers first used immortalized, TMZ-resistant cell lines implanted into the flank of mice with drug-resistant GBM. “With KL50, we observed a reduction in tumor burden without toxicity,” added Bindra. Next, the team implanted the cells into the brain tissue of the mice and observed the same efficacy without toxicity. “This was a very important result for us because CNS penetration is always a concern with these neuro cancers,” he added. Finally, large TMZ-resistant GBM tumors were implanted into the brains of mice and again KL50 achieved a significant reduction in tumor burden.
The team hopes to generalize on this approach to create new drug treatments that exploit a variety of DNA repair defects, not just those related to MGMT. “We are looking at other DNA damage repair defects that we think are clinically actionable for a range of different cancer types to obtain selectivity and we are making new classes of molecules,” says Herzon.
Though this concept was developed at Yale, Herzon and Bindra have formed a startup, Modifi Bio, that has been in stealth mode for two years until this Science paper was published to advance these types of compounds into the clinic. Their target is to initiate the first clinical trial in early 2024.













